Laser Precision
Focused laser energy delivers precision ablation in brain surgeries at Le Bonheur Children’s Hospital, allowing for improved outcomes and quicker recovery times for some patients.
Le Bonheur uses laser interstitial thermal therapy (LiTT) to address brain tumors and areas of the brain causing epileptic seizures that are hard to reach. The concept of LiTT has been around since the 1970s. But the therapy has emerged in the last 10 years as the technology, especially the probes used, became better and more reliable, according to Le Bonheur Neurosurgeon Nir Shimony, MD. He said open surgery is still a very important tool, but the laser gives patients more options.
How It Works
LiTT delivers focused laser energy to ablate the targeted brain tissue, including tumors or epilepsy areas. The laser is sent through a probe inserted through a small opening in the skull, about 3 millimeters wide. Using MRI guidance, neurosurgeons can monitor the ablation in real time, receiving updated images every eight seconds during the procedure. When a tumor or epilepsy is found, the laser does not remove the tissue, it destroys it.
“The idea of the laser, and it sounds very much like science fiction, but it’s actually just a way of transferring energy that will then become a heat or temperature-related energy that will get to a certain point that the protein is, basically, melted,” Shimony said.
To prepare for a LiTT surgery, Le Bonheur doctors meticulously map the source of seizures or tumors in the brain and what areas of the brain are required to preserve function using an advanced suite of brain imaging tools.

Using a 3 millimeter incision, Le Bonheur neurosurgeons can use laser ablation to destroy brain tumors and epilepsy areas. This minimally-invasive procedure can lead to better outcomes and quicker recovery.
For this, they use the Robotized Stereotactic Assistant (ROSA) One Brain. This robot has advanced software for mapping and guidance and a robotic arm that the software directs to precise, premapped locations. ROSA fits inside Le Bonheur’s neurosurgery Operating Rooms (ORs). ROSA makes procedures less invasive, shorter, improves surgical accuracy and minimizes the risk of pain or infection.
When preparing for a LiTT procedure, ROSA’s assistance begins before reaching the OR. Combining MRI, CT scans, and any other brain imaging from the patient, ROSA creates a comprehensive 3D map of the patient’s brain and head. Using these maps and ROSA’s software, neurosurgeons can create a plan for the trajectory of the electrodes so that they reach precise areas of the brain while avoiding critical structures.
Once in the OR, ROSA scans the patient’s facial features with a laser and matches the scan to the 3D map of the brain and head. ROSA then guides the surgical instruments to precise locations on the skull based on the surgical plan created before surgery. The extensive preoperative planning available with ROSA means the probe placement is highly accurate, as the robot guides instruments to their precisely planned locations.
For all of this, ROSA makes LITT procedures shorter, safer and with better outcomes for patients.
But LITT is not the right tool for every brain surgery. Large tumors and large treatment areas call for multiple laser probes, making surgeries very long, increasing risks involved with lengthy anesthesia.
Clinical Advantages
Compared to open surgery, LiTT offers a host of benefits, especially for patients with lesions deep in the brain or those with prior surgical scarring.
“The main improvement is how [patients] are doing after surgery,” Shimony said. “Most of the laser patients go home the next day or stay another night in the hospital. They feel very good because [surgeons] didn’t disrupt anything in their brain besides the lesion you want to destroy.”
LiTT could be ideal for patients who have had previous brain surgeries and any scar tissue that goes with them. Another open surgery risks injury or damage to normal tissue, Shimony said. LiTT allows for precise targeting of treatment points, bypassing any healthy or scarred tissue.
Real-Time Control and Ongoing Innovation
In the MRI control room, Le Bonheur surgeons like Shimony adjust the direction and depth of the probe as the procedure progresses, giving them accurate control with near-real-time feedback.
“You see it happen in front of your eyes,” Shimony said. “It’s like you’re in the brain [at the moment]. Then, you’re destroying the tissue, selecting it from the MRI picture. You get a new picture every eight seconds. So, it’s an ongoing process.”

Neurosurgeons use the ROSA One Brain technology to map the brain and head, develop a surgery plan and then guide surgical instruments to the precise location for a successful laser ablation.
Emerging innovations include smaller probes, some as small as 1.6 millimeters, about the size of the head of a pin, which will make the procedure even less invasive. Also, new technology will allow surgeons to determine what side of a probe surgeons can use to burn, not just using the entire cylinder shape, for even more control. All of this could make more feasible the possibility of those multi-probe procedures that now tend to take longer, Shimony said.
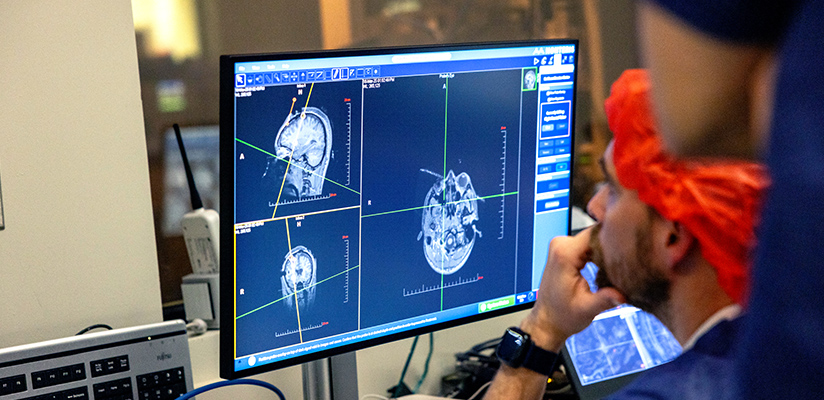
Laser ablation procedures are guided by MRI. Neurosurgeons watch the brain tissue destroyed in real time, adjusting the probe as needed.
A Regional Resource
Le Bonheur is one of the few pediatric hospitals in the southeast regularly using LiTT to conduct delicate surgeries for brain tumors and epilepsy centers.
“We are lucky here and have a unique situation,” Shimony said. “Memphis is in the junction between several states.
“I would say more than about half of our patients are not actually from here. So, people are coming from all over. And we are happy to help anyone who needs any kind of attention or help.”
Help us provide the best care for kids.
Le Bonheur Children's Hospital depends on the generosity of friends like you to help us serve 250,000 children each year, regardless of their family’s ability to pay. Every gift helps us improve the lives of children.
Donate Now






