Tackling tumors
Pediatric Neurosurgeon Frederick Boop, MD, has fought for improved survival rates for many of the pediatric brain tumors he has treated in his 30-year career. For most, he has witnessed great success.
But for one particularly aggressive type of tumor – pediatric glioblastoma – outcomes remain bleak. It remains a diagnosis he never wants to deliver. Those poor outcomes have pushed Boop and a team of researchers at the University of Tennessee Health Science Center (UTHSC) – led by cancer researcher Lawrence Pfeffer, PhD – to dig deeper into why these tumors are so resistant to treatment.
The key: cancer stem cells.
“When you think about brain tumors over my lifetime, we’ve gone from 30 percent five-year survival rates to 80 percent five-year survival rates for most brain tumors in kids. But with glioblastoma, we haven’t made tremendous progress in the outcomes,” said Boop, who serves as chairman of the Department of Neurosurgery at UTHSC, co-director of Le Bonheur’s Neuroscience Institute, and chief of Pediatric Neurosurgery at St. Jude Children’s Research Hospital.
Glioblastoma multiforme (GBM) is a rare high-grade glioma that arises from the brain’s glial cells. The aggressive tumors are difficult to treat in both children and adults and have some of the lowest survival rates. Only 20 percent of children with a GBM live five years or longer.
Within these tumors are cancer stem cells – the cells responsible for tumor initiation and growth. Isolating them is crucial for making new discoveries when it comes to GBM treatment, scientists believe.
“In the last decade, we’ve gained a much better understanding of the molecular genetics of the cells that make up these tumors,” said Boop. “One of the things we’ve learned is that not every cell in the tumor can keep growing and make a tumor.”
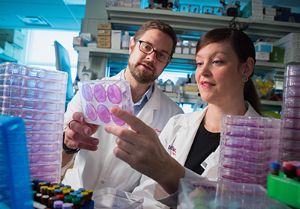
For the past two years, cancer researcher Pfeffer and his team have collected GBM tissue from Boop’s operating room, isolating the tissue’s cancer stem cells and growing them in the lab. They’ve built a repository of cultivated cancer stem cells that researchers can use to study new treatment therapies.
Pfeffer has already made one such discovery analyzing adult GBM tissue. Though GBMs are equally devastating in both adults and children, the disease responds differently to treatment in adults than it does in children. So the two must be studied separately, he says.
Hope with Ben

Fifteen-year-old Ben Leary’s headaches began on a Friday last October. Throughout the weekend, he complained of worsening pain. Even his sister’s prescription-strength migraine medicine couldn’t provide relief. By Tuesday, Penny Leary took her son straight to the emergency room.
“He said ‘mom, these headaches are killing me.’ He woke up at 4 a.m. and couldn’t go back to sleep,” said Penny. There, they learned that Ben had a brain tumor. Pathology later delivered another devastating blow. It was a pediatric glioblastoma – a particularly aggressive type of malignant tumor. Shortly after Ben’s diagnosis and emergency surgery close to home in New Orleans, La., Penny and her family felt a “pull” to go to Memphis for Ben’s care. After a phone conversation with Pediatric Neurosurgeon Frederick Boop, MD, the Learys were certain that was where Ben needed to be.
Memphis is home to one of the largest pediatric brain tumor programs in the country – a joint effort between St. Jude Children’s Research Hospital and Le Bonheur Children’s Hospital. The program began in 1985 and has grown to become one of the most reputable programs in the country – with state-of-the-art technology and groundbreaking research efforts.
“I felt a pull, a force guiding me to St. Jude,” said Penny. “Dr. Boop called me himself, and the moment I heard his voice, I felt a comfort, calmness within his voice.” This fall, Ben underwent another surgery at Le Bonheur Children’s, where Boop removed even more of his tumor. He began a seven-week radiation regimen in December at St. Jude. His family and friends sport bracelets that say “Hope with Ben” to show their support. They hope research will lead to cures for families like theirs. “The stories that we have come across, there is such sadness, confusion, loss for words, despair in each situation. I pray for each one of us. We are each asking for our miracle, our healing,” said Penny.
Help us provide the best care for kids.
Le Bonheur Children's Hospital depends on the generosity of friends like you to help us serve 250,000 children each year, regardless of their family’s ability to pay. Every gift helps us improve the lives of children.
Donate Now