A Surgical Solution
Le Bonheur tackles region's pediatric obesity problem
Nineteen-year-old Anjelica Evans spent eight years living with type 2 diabetes. She took four medications daily, including a dose of insulin four times the amount prescribed to most adolescent patients with diabetes.
Struggling with obesity since childhood, Evans tried for years as a teenager to shed the weight. At her heaviest, she weighed 337 pounds. She felt renewed hope after she enrolled in Le Bonheur’s Healthy Lifestyle Clinic in 2016, which specializes in helping children and teens with obesity. When she learned adolescent bariatric surgery was an option due to the severity of her obesity and serious health complications, she jumped at the chance. It could save her life.
Anjelica isn’t alone in her struggles with obesity. According to the National Survey of Children’s Health, sponsored by the U.S. Department of Health and Human Services, nearly four in 10 Tennessee children and teens are classified as overweight or obese. This means Tennessee is now No. 1 in the country for childhood obesity.
September will mark one year since Le Bonheur began offering adolescent bariatric surgery – the newest piece in the four-year-old Healthy Lifestyle Clinic. Now, the clinic is offering a comprehensive menu of options for children and teens in and around the Memphis area struggling with obesity.
A valuable weight loss tool
Bariatric surgery became more widely available for teens in the early 2000s, and recent studies have shown that the operation is a safe and effective way to lose weight and improve health.
Teen-Longitudinal Assessment of Bariatric Surgery (TEEN-LABS), a research consortium of five clinical centers founded in 2007, has published numerous studies on the short- and long-term outcomes of bariatric surgery in adolescents. Its findings present a case in favor of surgery for extreme adolescent obesity – results that show improved quality of life and lower rates of diabetes and other obesity-related comorbidities.
“We know that obesity is linked to serious health complications, including obstructive sleep apnea, heart disease, hyperlipidemia, fatty liver disease, hypertension, diabetes and orthopedic issues,” said Ying Zhuge, MD, a pediatric surgeon at Le Bonheur who leads the Adolescent Bariatric Surgery program.
Zhuge received her medical and residency training at University of Miami and her pediatric surgical fellowship at Le Bonheur “Bariatric surgery is a valuable tool for some of our patients, and the benefits far outweigh the risks.”
Zhuge has performed six bariatric surgeries at Le Bonheur so far and is on track to complete another five by the end of 2018. She performs the laparoscopic sleeve gastrectomy, which is a restrictive procedure that reduces a patient’s stomach size by 85 percent. By shrinking the stomach, patients eat less, and hormones that control hunger are suppressed.
Anjelica underwent her gastric sleeve surgery at Le Bonheur in April and lost 18 pounds in the first three weeks. In the first week after surgery, her glucose levels dropped significantly, and she was able to reduce her diabetes regimen to only one medication. Doctors expect her to be able to drop that medication, too, with proper diet and exercise as she loses more weight.
“I believe her self-esteem will improve now that we’ve had the surgery,” said her mom, Joann. “We will see the real, true Anjelica.”
Joann, too, underwent a sleeve gastrectomy in 2013. The operation helped her lose 114 pounds. As a nurse who cares for adult patients with diabetes, Joann knew what a future without weight loss looked like for Anjelica.
“For years I worried about her and knew that if we didn’t get (her diabetes) under control, she would eventually lose a limb, have to undergo dialysis or have heart failure,” she said.
To qualify for bariatric surgery, patients must have reached skeletal maturity – which happens at about age 14 for girls and 16 for boys. They must also have a body mass index (BMI) of 40 or higher or a BMI of 35 or higher with at least one comorbidity, which includes obstructive sleep apnea, pseudotumor cerebri, hypertension, hyperlipidemia, fatty liver disease and type 2 diabetes.
Before the surgery, patients visit the Healthy Lifestyle Clinic routinely for at least six months to learn about potential complications of surgery, post-surgery recovery, medications, diet and exercise. After surgery, patients follow-up regularly at one week, three weeks, seven weeks and 11 weeks after surgery for post-surgical check-ups and dietitian counseling. Patients advance gradually to regular foods and, once they reach a regular diet, follow-up in clinic regularly at intervals that vary from every three months to annually, depending on how far removed they are from surgery.
“All of our bariatric surgery patients have been recommended based, not only on their weight and health criteria, but also on their history as reliable, responsible patients in our Healthy Lifestyle Clinic,” says Zhuge.
One size does not fit all
The bariatric surgery program rounds out the Pediatric Obesity program, jointly sponsored by Le Bonheur and the University of Tennessee Health Science Center (UTHSC). The obesity program is supported by grants from Memphis Urban Child Institute.
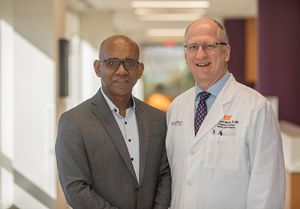
In 2014, Le Bonheur recruited a leading physician and researcher in the field of pediatric obesity medicine, Joan Han, MD. Han, who received her training at Harvard Medical School and the National Institutes of Health, has spent her career working to understand why some children struggle to maintain a healthy weight and others do not. At Le Bonheur and UTHSC, she’s developed a program that targets a patient’s root cause for obesity and creates an individualized treatment plan for each child.
The program has three main components: community-based wellness programs, a metabolic research center and a multidisciplinary clinic.
”We are addressing the pediatric obesity epidemic at multiple levels. Our community programs are aimed at obesity prevention by educating children and their parents about healthy nutrition and physical activity. Our research focuses on finding treatments for obesity that target specific genetic and other biologic factors. Our clinic combines these two approaches. We help patients develop life-long healthy habits and provide obesity treatments individualized for each patient’s needs,” said Han.

At the heart of the program is its Healthy Lifestyle Clinic, which has treated more than 900 children and adolescents since 2014. Each patient undergoes an initial evaluation by the program care team, which includes physicians, nurses, a dietitian, exercise physiologist, occupational therapist and behavioral psychologist. From there, a personalized health plan is developed. Plans could include any combination of diet changes, medication, exercise and behavioral therapy. And now – surgery.
Many adult studies, both prospective and randomized, have demonstrated that bariatric surgery, combined with intensive medical therapy, is superior to intensive medical therapy alone – both in the amount of weight lost and remission of obesity-related comorbidities. TEEN-LABS has led the way to conclude the same results for the adolescent population.
“Although the follow-up is shorter for adolescent studies — three years versus 12 for some adult studies — the dramatic improvement in weight, BMI, quality of life and resolution of major comorbidities cannot be argued,” said Zhuge.
Of the six patients who’ve undergone bariatric surgery at Le Bonheur, all have come through the Healthy Lifestyle Clinic. While their metabolic health improved in the clinic with lifestyle changes, surgery was still necessary because of the severity of their obesity and obesity-related comorbidities.
“For patients with severe obesity, lifestyle efforts can have initial success, but often there is a plateau in weight loss because the body’s internal drive to regain weight is so strong. Bariatric surgery can change the body’s physiology to allow for further weight loss and maintenance of that weight loss,” said Han.
Individualized treatment is key for pediatric obesity, says Han. After all, the causes of obesity, including genetic, behavioral and environmental factors, are complex – and weight isn’t the only issue at stake. Obesity causes myriad other health complications.
“We know in this field that one size does not fit all when it comes to treatment,” said Han. “And weight loss is not the only goal. We also want to improve body composition, metabolic complications, sleep quality and the child’s overall physical and mental well-being.”
Next steps
Han’s program has drawn patients from across the Mid-South region, and both Han and Zhuge anticipate that the addition of bariatric surgery will further increase interest in the program.
Anthony Sheyn, MD, a Le Bonheur pediatric otolaryngologist, treats several patients with obesity-related obstructive sleep apnea (OSA). He says adding bariatric surgery as an option for patients with severe obesity is important.
“Although OSA is often treated with CPAP or upper airway surgery, weight management in overweight and obese children is a very important part of treatment. OSA is curable, and can be preventable, when weight loss is coupled with other treatments,” he said. “Our bariatric surgery team allows our facility to offer complete care to these patients and is a great option to offer our patients who have otherwise struggled with weight loss.”
As far as next steps for the program, Zhuge hopes to apply for accreditation by the Metabolic and Bariatric Surgery Accreditation and Quality Improvement (MBSAQI) program in the next few years, as volumes increase. To date, only 6 centers have earned the MBSAQI’s adolescent accreditation – a stamp of approval for quality programs. She also hopes to form a Mid-South collaborative with other centers in the region who offer adolescent bariatric surgery. Doing so, she says, will allow physicians to study the Mid-South’s adolescent bariatric surgery patient population, which looks much different than those reflected in the major studies published by TEEN-LABS.
Childhood obesity is clearly still a big problem in the region, and the Le Bonheur/UTHSC Pediatric Obesity program plans to continue its efforts and tackle the issues at stake.
“Obesity rates have more than tripled since the 1970s,” said Han. “It took a generation to get us to this point, and it may take a generation to reverse this epidemic. Le Bonheur’s Healthy Lifestyle Clinic continues to strive toward this goal, one patient at a time.”
Help us provide the best care for kids.
Le Bonheur Children's Hospital depends on the generosity of friends like you to help us serve 250,000 children each year, regardless of their family’s ability to pay. Every gift helps us improve the lives of children.
Donate Now