Program Overview
The Pediatric Psychology Fellowship at Le Bonheur/UT Health Science Center aims to provide advanced training in clinical service, scholarly inquiry, professionalism and ethical decision-making. The program is committed to advancing the profession of psychology and maximizing child health outcomes through exemplary postdoctoral training. Fellows will gain experience in a variety of pediatric subspecialties and develop the skills necessary to work in pediatric health care settings and/or university-based training programs.
This fellowship adheres to the Association of Psychology Postdoctoral and Internship Centers (APPIC) standards for postdoctoral training, including structured supervision and a planned sequence of training experiences. Supervising psychologists within this track include Patricia Logan, PhD, ABPP, Adrienne Arrindell, JD, PhD, Gwen Beard, PsyD, William Dalton, PhD, and Donald Bearden, PhD, ABPP-CN.
We invite applications for a one-year fellowship in pediatric psychology. Pediatric psychology fellows engage in various clinical activities within interdisciplinary outpatient clinics and inpatient settings, including consultations with social workers, nurses and physicians. Pediatric psychology fellows spend approximately 50% of their patient contact hours as primary clinicians for long- and short-term individual therapy cases involving children and adolescents, as well as cases requiring parent behavior management training. Fellows will manage a range of internalizing and externalizing psychological disorders affecting children and families across all age ranges. The remaining 50% of the patient contact hours are dedicated to psychological assessment. Referral questions typically include learning disorders, ADHD and diagnostic clarification of other behavioral and emotional difficulties. Evaluations involve evidence-based assessment strategies and often focus on objective testing of cognitive, academic and emotional/behavioral functioning.
Learn more about how to apply.
Salary and Benefits
-
The current annual stipend for the fellowship is $68,000
-
As employees of The University of Tennessee Health Science Center (UTHSC), a comprehensive benefits package is provided.
-
Fellows time off includes UTHSC's official holiday schedule (~12 holidays plus winter closings). Fellows also accrue annual leave at 16 hours per month and sick leave at 8 hours per month in accordance with UTHSC staff policy.
-
Other benefits include free lunch in Le Bonheur's Physician Dining Hall, free parking, full access to library resources, administrative support and study materials for the Examination for Professional Practice in Psychology (EPPP).
Pediatric Psychology Training Rotation
Approximately 70% of the fellow’s time is spent in clinical activities, 10% in didactics and supervision and 20% in research. Le Bonheur’s pediatric psychology fellowship program offers specialized training rotations to cater to the diverse interests and career goals of fellows. These rotations include:
Rotation in Interdisciplinary Eating Disorders Clinic
Supervised by Adrienne Arrindell, PhD, JD, this rotation provides fellows with hands-on training in a collaborative, team-based setting that serves children with complex developmental, medical, nutritional and behavioral needs. The clinic brings together professionals from medicine, nursing, nutrition, occupational therapy and psychology, offering fellows a rich opportunity to engage in integrated care.
All clinicians work in a shared central space, allowing for real-time discussion of each patient and collaborative decision-making regarding which providers are most appropriate for a given visit. This structure fosters a dynamic and responsive approach to care, with new patients seen during nearly every clinic session and typically evaluated by all providers. Fellows participate in these assessments, rotating not only with the psychologist but also with other disciplines to gain a comprehensive understanding of patient needs and interdisciplinary care.
- Fellows will learn how to implement Family Based Treatment for Eating Disorders, the first line, evidence-based treatment for youth with these conditions.
- Due to limited capacity for ongoing psychological therapy within the clinic, many patients are referred to community mental health providers for continued care. However, some patients are seen regularly in the clinic for therapy, and fellows may assist in this care and potentially develop a small caseload depending on their experience and availability. Fellows will contribute to brief interventions focused on behavioral regulation, family support and adjustment to developmental or medical challenges. Supervision is primarily conducted in real time, with the attending psychologist present during all patient contact. Fellows also engage in collaborative case formulation and documentation, receiving guidance and feedback throughout the clinical process.
- The rotation emphasizes responsive, family-centered care and provides fellows with experience in developmental screening, behavioral assessment and interdisciplinary consultation. Fellows will learn to incorporate social determinants of health into care planning and may participate in school consultations or referrals to community services. Didactic opportunities may include seminars on feeding and nutrition, trauma-informed care, interdisciplinary models and systems-level approaches to pediatric health. Optional involvement in clinical research or quality improvement initiatives related to developmental medicine may be available.
- The rotation typically lasts four to six months, with flexibility depending on the structure of the fellowship program. Fellows dedicate one to two days per week to the clinic, including patient care, documentation and supervision. A minimum supervision ratio of one hour for every four to five hours of direct patient contact is maintained, with additional informal supervision during clinic hours. Fellows are evaluated on their clinical skills in assessment and intervention, professionalism in interdisciplinary collaboration, integration of psychological and medical knowledge and use of culturally competent, family-centered approaches. Contributions to documentation, care planning and any programmatic or research initiatives are also considered in the evaluation process.
Rotation in Congenital Heart Defects (CHD)

Supervised by Patricia Logan, PhD, this rotation offers advanced training for fellows in the psychological assessment and intervention of children, adolescents and families affected by congenital heart defect (CHD). This rotation emphasizes the development of expertise in psychosocial, developmental and family systems issues related to complex cardiac conditions, surgical procedures and long-term disease management. Fellows work within a multidisciplinary medical team and are trained in evidence-based psychosocial interventions and culturally responsive practices to support diverse patient populations.
- Throughout the rotation, fellows are expected to demonstrate advanced knowledge of the medical, neurodevelopmental and psychosocial sequelae of CHD across developmental stages. They will conduct psychological assessments, including screening, diagnostic, neurocognitive and behavioral evaluations, and deliver both brief and extended interventions focused on adjustment, treatment adherence, procedural anxiety, emotional regulation and family coping. Fellows collaborate closely with cardiologists, surgeons, nurses, social workers and rehabilitation specialists, integrating an individual’s background and situation into care planning. They also consult with schools and community providers to support the educational, behavioral and social needs of children with CHD, and participate in program development, research and quality improvement initiatives.
- Clinical activities include providing family-centered interventions to promote adherence, stress management and resilience; leading psychoeducation groups for parents and siblings; and developing care plans for common concerns such as procedural anxiety, sleep disturbances and cognitive or learning challenges. Fellows offer consultation-liaison services for hospitalized patients undergoing cardiac procedures and collaborate with cardiology and intensive care teams on discharge planning, outpatient transitions and school reintegration.
- Supervision and didactic training are integral to the rotation. Fellows receive weekly one-on-one supervision from a pediatric psychologist specializing in CHD and attend pediatric cardiology case conferences, morbidity and mortality reviews and interdisciplinary rounds. They also participate in seminars covering cardiac physiology, developmental outcomes, adherence, grief and loss and trauma-informed care, with optional involvement in clinical research or quality improvement projects.
- The rotation typically lasts four to six months, with a flexible structure depending on the fellowship program. Fellows dedicate two days per week to CHD services across inpatient, outpatient and consult-liaison settings, with a minimum supervision ratio of one hour for every four to five hours of direct patient contact. Evaluation criteria include clinical skills in assessment, intervention and consultation; integration of psychological and medical knowledge; professionalism in interdisciplinary collaboration;, family-centered approaches; and contributions to programmatic, research or quality improvement efforts.
Rotation in Neurology & Neuropsychology

During the neurology rotation supervised by Gwen Beard, PsyD, pediatric psychology fellows gain valuable experience working within interdisciplinary medical teams, with a focus on supporting children and adolescents with neurological conditions. A key component of this rotation includes consultation-liaison services on the Epilepsy Monitoring Unit (EMU), where fellows collaborate with neurology, nursing and other medical staff to provide psychological support to patients undergoing diagnostic evaluation and seizure monitoring. Fellows conduct brief bedside assessments, provide psychoeducation to families and assist with coping strategies and behavioral management during hospitalization.
- In addition to consultation-liaison work, fellows engage in comprehensive psychological assessments for children referred through neurology for concerns related to learning disorders (LD), attention-deficit/hyperactivity disorder (ADHD), autism spectrum disorder (ASD) and other neurodevelopmental or behavioral conditions. These evaluations involve clinical interviews, standardized testing and integration of medical and educational history to inform diagnostic impressions and treatment recommendations. Fellows receive supervision in test selection, administration, scoring and report writing, with an emphasis on tailoring assessments to the unique needs of medically complex pediatric populations.
- This rotation provides fellows with opportunities to develop clinical competencies in neurodevelopmental assessment, interdisciplinary collaboration and family-centered care within a pediatric neurology setting. Additionally, fellows receive specialized training in Comprehensive Behavioral Intervention for Tics (CBIT) under the supervision of a CBIT-certified psychologist. This training includes didactic instruction, case-based learning and supervised clinical practice, equipping fellows with evidence-based skills for treating tic disorders within pediatric populations.
Clinical Training
Fellows will participate in clinical assessment and intervention experiences across various pediatric populations. Clinical skills development is supported by ongoing formal and informal didactics, ensuring fellows are well-prepared to provide care for diverse pediatric populations.
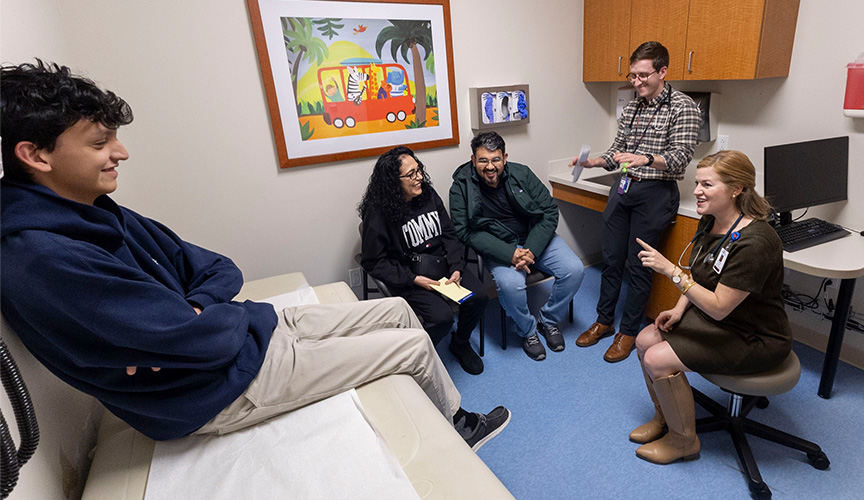
Interdisciplinary Collaboration
Fellows will work with interdisciplinary teams, including physicians and social workers, to deliver comprehensive mental health care to patients admitted to medical units. Fellows will also provide mental health training to other health care professionals, emphasizing the importance of collaboration in delivering comprehensive care.
Supervision and Teaching
Fellows will have opportunities to supervise practicum students and other trainees, collaborate in interdisciplinary treatment teams, and participate in care coordinated across multiple specialty services. They will also provide educational opportunities to other professionals in the healthcare system, enhancing their teaching and supervisory skills.
Programmatic Care and Development
Fellows will gain exposure to programmatic care along with the development of programs and systems of care. They will be responsible for working with interdisciplinary teams and patients referred to various service areas, contributing to the development and implementation of effective care programs.
Competency Evaluation
The development of increasing competence is evaluated informally through supervision and formally through written evaluations every six months. Fellows are given increasing clinical responsibility, autonomy and exposure to more challenging treatment cases as they demonstrate readiness, ensuring their growth and development throughout the fellowship.
Ethical and Professional Conduct
Fellows will receive training in professionalism, ethical decision-making and legal matters. They are expected to conduct themselves professionally and build interpersonal relationships, adhering to the highest standards of ethical and professional conduct.
Research and Scholarly Inquiry
Fellows are offered opportunities for scholarly inquiry and are trained in research methods and systems evaluation. They are encouraged to contribute to the field of psychology through clinical work, research and education, fostering a culture of continuous learning and innovation.
Specialized Applied Experience
Fellows will train across a wide range of medical subspecialties. They will conduct initial evaluations, consultations and psychotherapy, gaining valuable applied experience in various clinical settings.
These components aim to provide a comprehensive overview of the fellowship program, ensuring that prospective fellows have a clear understanding of the training, experiences, and opportunities available to them. Training objectives are customized for each specialization with a varied emphasis on clinical and research elements. Each specialization has a training lead responsible for overseeing the fellow's training plan, including licensure preparation. All fellows take part in didactics that focus on professional development, cultural competency, clinical/research training and licensure.
Pediatric Psychology Common Hold Date
We are in the process of applying for Association of Psychology Postdoctoral and Internship Centers (APPIC) membership; this is pending approval. For the upcoming fellowship year (2026–27), we will accept applications outside of APPIC. Therefore, applicants must obtain a provisional license from the Tennessee Board of Examiners in Psychology before beginning clinical work. The provisional license is valid for one year and may be extended upon request if additional time is needed to complete supervised hours. Fellows will be reimbursed for costs associated with obtaining their provisional license.
Applicants for the Pediatric Psychology track should have a strong foundation in child and pediatric psychology, with training in evidence-based interventions for children and families. Preferred qualifications include:
- Clinical Competence: Experience providing evidence-based therapy (e.g., CBT, ACT, family interventions) for children and adolescents in medical or behavioral health settings.
- Assessment Skills: Proficiency in psychological assessment of emotional, behavioral and developmental concerns, including risk assessment and diagnostic formulation.
- Medical Integration: Interest in working within pediatric health care teams, addressing psychosocial adjustment to chronic illness, adherence and coping.
- Cultural Context: Experience serving varied and underserved populations, with sensitivity to an individual’s background.
- Interdisciplinary Collaboration: Ability to work effectively with physicians, nurses, social workers and other professionals in multidisciplinary care.
- Professional Development: Commitment to ethical practice, scholarly inquiry and preparation for licensure as a health service psychologist.



