A New Standard
Le Bonheur Pediatric Surgeon Tim Jancelewicz, MD, recently conducted a systematic review of papers addressing the management of pilonidal disease, showing that less invasive management should be first-line treatment, and wide excision should no longer be the management of choice except possibly in the case of recurrent or chronic disease.
The research was published in Journal of Pediatric Surgery on behalf of the American Pediatric Surgical Association Outcomes Committee. The aim of the study was to develop clinical practice guidelines for surgeons regarding the management of the disease based on the best available evidence.
“To date there have been no comprehensive guidelines for the management of pilonidal disease,” said Jancelewicz. “With these guidelines, we can give the best care up front in order to minimize the risk of recurrence, avoid maiming operations and minimize the patient’s time away from school or work.”
Pilonidal disease (PD) is a common and often debilitating infectious and inflammatory condition of the gluteal cleft and sacrococcygeal region characterized by sinus and abscess formation. Recurrence is common, and the peak ages affected by the disease are between 15 and 22 years. For decades the standard definitive care has been excision with either secondary healing or primary closure of the wound, but recurrence is very common. PD is painful, debilitating and embarrassing for adolescents and young adults. The ideal approach to treatment would minimize pain and suffering and have low recurrence rates.
The study reviewed 193 articles between 1965 and June 2017 that addressed the operative or nonoperative management of PD. The review excluded cases before 1964, low quality and irrelevant articles. The following questions were asked during the systematic review:
- Are non-operative and minimally invasive management strategies effective treatment for pilonidal disease?
- What are the indications, contraindications and associated complications with various operative techniques for pilonidal disease?
- What operative and non-operative approaches for the treatment of pilonidal disease are associated with the highest quality-of-life and patient satisfaction?
Various methods of intervention for PD were reviewed. Non-operative procedures include standard hair removal and hygiene, laser hair removal, phenolic acid and fibrin glue. Minimal surgery techniques included incision and drainage, minimally invasive pilonidal excision (MIPE), sinusectomy and endoscopic approaches. Finally, the study reviewed the use of excision or removal of affected tissue with en bloc resection. This has been the most common definitive surgical treatment of PD for decades.
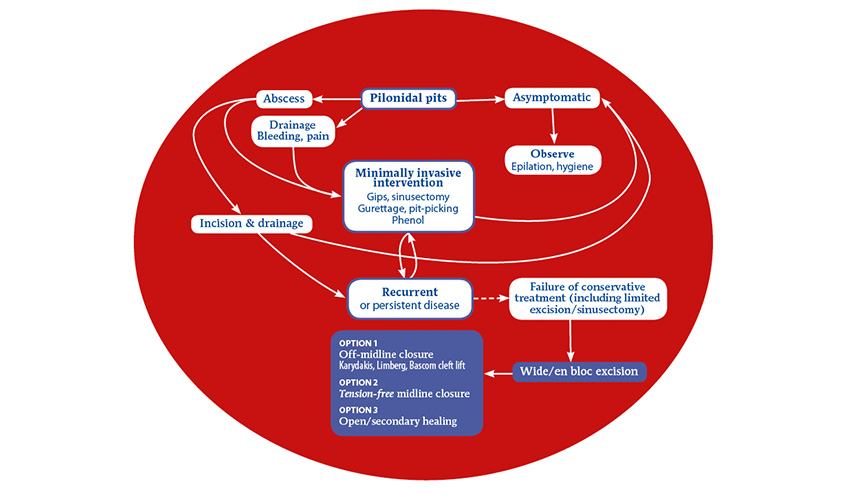
The review identified that there has been a clear trend towards less invasive management because of unacceptably high failure rates seen after traditional wide excision and patient preference of less invasive procedures. The study created a management algorithm for PD that recommends minimally invasive intervention unless PD is recurrent or chronic.
“It is crucial to have guidelines for the pediatric surgeon because we often see pilonidal patients at their first presentation,” said Jancelewicz. “Minimally invasive pilonidal excision should be used as a first approach – it is safe, effective and much easier for both the patient and surgeon.”
Help us provide the best care for kids.
Le Bonheur Children's Hospital depends on the generosity of friends like you to help us serve 250,000 children each year, regardless of their family’s ability to pay. Every gift helps us improve the lives of children.
Donate Now















