Transcranial magnetic stimulation (TMS) is a non-invasive way that Le Bonheur physicians can look at and map the brain to find the areas that control language and movement. Generally, TMS is used for patients with epilepsy or a brain tumor who will undergo surgery. The maps from TMS help physicians to plan the surgery to keep as much language and movement function as possible and provide a reference point for any changes that occur in these functions after surgery.
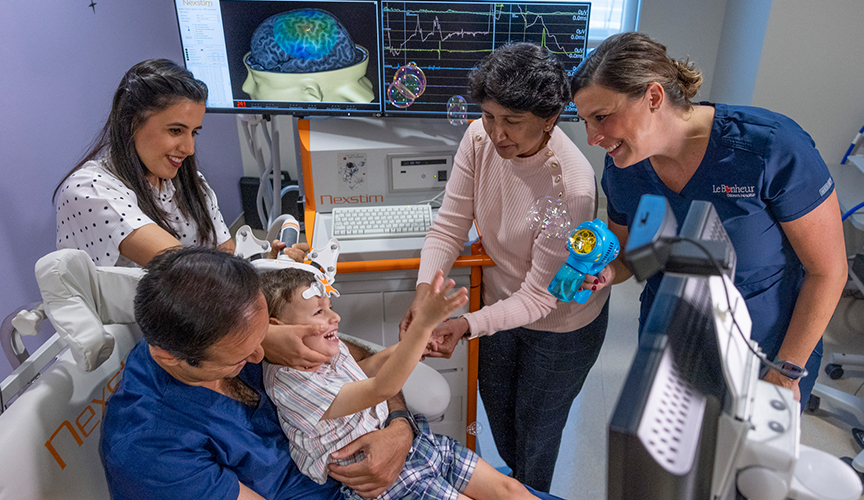
The technology uses the patient’s MRI to guide the TMS scan. TMS works by using a wand-like device on the outside of the head to stimulate the brain with a gentle tap through a magnetic field. The process is comfortable and painless for all ages. No sedation is ever used, and patients sit in a comfortable chair throughout the process. Small children can even sit in a caregiver’s lap.
Transcranial magnetic stimulation (TMS) is just one piece of the suite of technologies that Le Bonheur’s Neuroscience Institute uses to map the brain. Le Bonheur is one of the first children’s hospitals to use this brain mapping technology in clinical care and research. Le Bonheur uses the Nexstim Navigated Brain Stimulation (NBS) system, which was funded by the Shainberg Neuroscience Research Fund at Le Bonheur.
Benefits of Transcranial Magnetic Stimulation (TMS)
- Transcranial magnetic stimulation (TMS) can test expressive language, the ability to speak and communicate, which cannot be mapped using fMRI or MEG (magnetoencephalography) scans.
- Children are never sedated, and TMS does not require a patient to remain still.
- All ages can undergo testing with TMS, from young children to adults.
- TMS is completely non-invasive and painless.
- Even when patients aren’t able to fully cooperate due to disease or developmental delay, TMS testing is still possible.
Why Le Bonheur’s Transcranial Magnetic Stimulation (TMS) Program?
- Because of our expertise, we are able to complete TMS scans quickly. Typically, the process takes less than two hours because our experts know exactly what to look for thanks to their extensive experience using TMS.
- A child life specialist is available to explain the test in detail to each child and help make sure they are comfortable during the duration of TMS.
- We provide TMS scans for patients of all ages, including adults.
- The TMS program is part of a larger suite of brain mapping technologies in the Neuroscience Institute. Using these multiple techniques for identifying crucial function areas leads to the highest level of accuracy and planning for surgery.
- Our neuroscientists are able to provide a quick turnaround of results to referring physicians, often within days of the TMS scan.
- Le Bonheur’s TMS experts are some of the foremost in the field of neuroimaging. Le Bonheur Director of the TMS Laboratory Shalini Narayana, MS, MBBS, PhD, has published numerous papers showing the safety and efficacy of TMS in children.
Undergoing Transcranial Magnetic Stimulation (TMS)
- Patients sit in a comfortable chair (similar to a dentist’s chair) that is adjustable. Small children can also sit in a parent’s lap.
- A child life specialist is available to explain the TMS process to children and provide distraction throughout the scan if needed.
- A small tracker is placed on the forehead that allows neuroscientists to align the 3D model of a patient’s fMRI with the head. This enables the clinician to see exactly where TMS will stimulate the brain.
- Using a wand like device, a coil of wiring creates a magnetic field that causes a small electric field to pass harmlessly through the skull and into the brain to stimulate different areas. This electric field prompts the neurons of the brain into action allowing neuroscientists to identify the various areas of the brain where speech and motor function live.
- In order to determine the areas of the brain responsible for speech, patients are first shown pictures of everyday objects to name.
- Patients are then shown the same set of pictures with stimulation by moving the coil around the head. If a patient hesitates or loses the ability to speak when shown a picture while under stimulation, neuroscientists know they have found an area of the brain that is vital for speech.
- Any interference to speech only lasts a few seconds and is harmless to the patient.
- Neuroscientists will match the stimulation locations to changes in speech to map the vital areas of the brain for speech.
- If the brain is stimulated in an area responsible for movement, it will cause the associated muscle to move.
- In order to find these areas, neuroscientists start by finding the area of the brain that controls the thumb muscle. Once this area is found, clinicians determine how low the stimulation can be while still making the thumb move. This allows for a personalized scan that is reliable for mapping but comfortable for the patient.
- Electrodes are placed on the skin over the muscle that the neuroscientists wish to study. These muscles are chosen based on where the brain tumor or area for epilepsy surgery is located.
- As the clinician moves the coil over the head, any areas of motor function will cause the associated muscle to activate.
- Neuroscientists then match the locations of the brain that caused a muscle to move in order to identify the areas of the brain that control movement.





