Big Strides for Little Lungs
Le Bonheur Children’s Neonatal Intensive Care Unit (NICU), the region’s only Level IV NICU, was looking for an innovative way to care for one of its growing patient populations — babies with severe bronchopulmonary dysplasia (BPD). When plans began for an expansion to the hospital, Neonatologist Mark Weems, MD, medical director of the NICU, saw an opportunity. With the new space, Le Bonheur could cohort this population of patients with unique needs with the potential to improve their care and advance BPD treatment strategies by leaps and bounds.
BPD is a chronic lung disease found in premature babies that affects up to 43% of this population, according to the BPD Collaborative – a group of physicians and centers dedicated to fostering research of and treatment options for this population. Le Bonheur joined this collaborative in 2023 partnering with more than 45 other health centers. The need for interdisciplinary BPD programs, like Le Bonheur’s, are vital to improve survival and outcomes and decrease hospital stays.
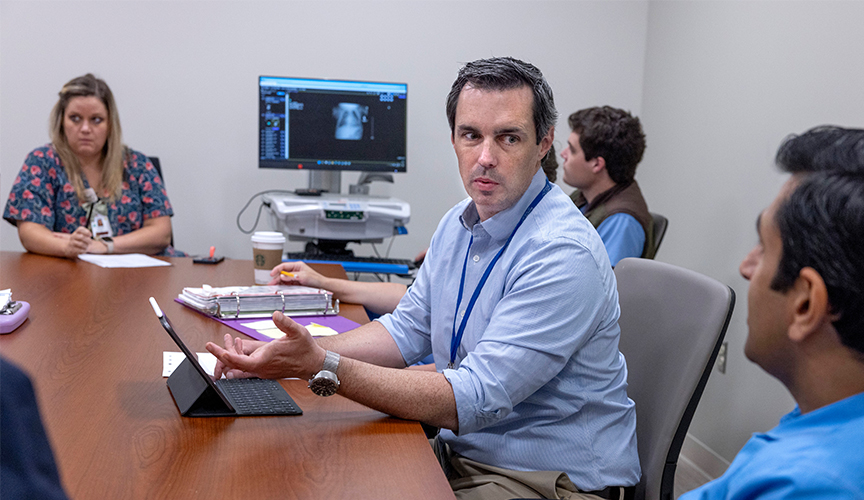
Mark Weems, MD, medical director of Le Bonheur’s NICU, leads the dedicated care team for BPD patients. This group consists of neonatologists, pulmonologists, cardiologists, rehab specialists and therapists as well as myriad support services for patients and families in the BPD unit.
Recently, Weems joined other members of the BPD Collaborative to publish recommendations in The Journal of Perinatology on how to develop a multidisciplinary BPD program. The article covered the basics of forming a program, growth strategies and the role of dedicated BPD centers in research.
Le Bonheur is one of a few centers to have a multidisciplinary team of providers and a dedicated space for this patient population. Thanks to this NICU expansion, known as the Center for Lung Development, Weems and the BPD team have seen improved survival and reduced tracheostomies among patients with severe BPD.
The Need
Premature infants are born with lungs that are not fully formed, which can lead to impaired development of the growing lungs. Some premature babies can require oxygen and respiratory support, which can further injure the lungs. BPD can occur due to either of these factors or a combination of both.
The article from Weems and the BPD Collaborative highlighted some of the challenges in this patient population that an interdisciplinary BPD center, like Le Bonheur’s, could help mitigate. These include maintaining continuity of care among providers, minimizing variations in patient management, lack of staff knowledge in developmental care for older infants and lack of evidence for specific therapies for BPD.
“There is an increasing need for strategies to improve chronic management of this complex patient population within an acute care setting,” the authors say. “To meet this need, interdisciplinary BPD programs have been developed…to improve survival, decrease hospital length of stay and costs, improve neurodevelopmental outcomes and facilitate the transition from the hospital to the outpatient setting.”
At Le Bonheur, the start and expansion of the BPD program began in 2019 when Weems and other providers in the NICU recognized that babies were surviving earlier gestation, but more patients were diagnosed with BPD and had poor outcomes.
Through the years, the program has grown, says Weems, adding elements over time, including weekly patient reviews, nutritionists, rehabilitation specialists, physical and occupational therapists, as well as specialists in neonatology, cardiology, pulmonology and more.
“With the expansion, we had the idea to take another step in the management of these patients and cohort them into a single team area,” said Weems. “This is unique among NICUs but has allowed us to decrease variability in care practice and establish dedicated nursing care.”

The Roadmap
The keys to a BPD program start with a multidisciplinary staff and providers, consensus guidelines for medical management and a defined scope of care, says the article from Weems and the BPD Collaborative.
“The established BPD program can and should evolve into a program that develops innovative approaches to BPD that are then adopted by early- and middle-stage programs,” say the authors. “The team’s ongoing goal should be to continue to standardize BPD care by applying any new evidence that becomes available.”
The authors place special emphasis on clear messaging and frequent communication with parents and caregivers. Support services, such as social workers or case managers, can also encourage parent engagement and bridge any communication gaps with providers.
The final piece of a multidisciplinary BPD program is an emphasis on research collaboration with the goal of standardizing BPD care, say the authors. Some of the keys that the BPD Collaborative identified are maintaining a data repository to track patient outcomes, quality initiatives to advance and refine practices and participation in national BPD organizations to compare outcomes.
“To prevent BPD, we need to learn how to wean babies off ventilators sooner and prevent damage from occurring,” said Weems. “But for babies who already have lung injury, the next steps are better understanding how we get the lungs to grow optimally going forward. This is where the BPD Collaborative’s work is essential.”
The Program
Le Bonheur’s BPD Program with the Center for Lung Development is one of the leaders among NICUs around the country in implementing these best practices. At Le Bonheur, this patient population now has a primary care team dedicated solely to them – not just a consult service. This currently consists of six dedicated neonatologists plus pulmonologists, cardiologists, rehab specialists and therapists, as well as support from a clinical nurse leader coordinator and data support specialist.
Weems and the team also strive to not only provide the best care to patients but support parents and caregivers of these infants through a parent support group, child life specialists, social workers, a psychologist and a discharge planner. Patients are discharged into Le Bonheur’s Complex Care Clinic for management and have follow up at multiple specialty clinics, including the dedicated BPD Clinic.
“We have improved survival and reduced tracheostomies by about 40% since the launch of our BPD program due to optimal nutrition, non-invasive ventilator support and consistency of care,” said Weems.
The Center for Lung Development in the NICU contains features designed for the unique needs of these infants and their caregivers. For older infants who have lived in a hospital room their entire lives, the Infant Development Room provides a new space for new experiences. In this room, they can interact with family members, meet a therapy dog or have interactions with other children who have had long-term stays in the NICU.
Also on the unit is the Caring Transitions Room – a place for parents and caregivers to practice overnight care for their child in the comfort of the hospital. The room is set up with a bed and amenities for families to practice the overnight medical care they need to master before discharge.

The Future
Opportunities to advance the care of children with BPD are plentiful, says Weems. His article with the BPD Collaborative states that participating in national organizations with shared knowledge are already moving the needle on successful care of this population. These multicenter collaboratives are vital, the authors state, because “comprehensive standardization, data collection and rigorous evaluation of approaches are needed to evaluate therapeutic effectiveness.”
Research initiatives around this population continue in Le Bonheur’s NICU. Two upcoming research efforts are to evaluate neurodevelopment support practices as well as the efficacy of zinc supplementation. Weems also plans to continue to develop the BPD program as a whole with two immediate goals of increasing family education and adding a case manager to their team.
“One of our future goals is participate in developing consensus with other centers on the optimal trach recommendation and additional care practices for BPD patients,” said Weems. “Our dedicated unit is unique among NICUs, and we will continue the process of improving survival and reducing length of stay and tracheostomies for these infants.”
Help us provide the best care for kids.
Le Bonheur Children's Hospital depends on the generosity of friends like you to help us serve 250,000 children each year, regardless of their family’s ability to pay. Every gift helps us improve the lives of children.
Donate Now