Brain Tumors and Epilepsy
Seemingly unsolvable medical mysteries about a child’s seizures often land at Le Bonheur Children’s Hospital.
Families arrive after skilled neurologists across the country exhaust their options, knowing Le Bonheur’s national reputation for unraveling complicated puzzles, especially around children who have epilepsy and brain tumors simultaneously. For those families, their comprehensive search for answers for their children often ends in Memphis.
Brain tumors and seizures can both be life-threatening and devastate a child’s quality of life. When those powerfully destructive diagnoses present together, the mystery runs deep, often with complicated answers. That’s when Le Bonheur’s expert-led pediatric programs — neurology, neurosurgery, neuroradiology and more — join forces to fight back in a united front.
The Patient Path

for patients with simultaneous epilepsy and brain tumor. Pictured here are members of the team (left to right),
Le Bonheur and Semmes Murphey Neurosurgeon Nir Shimony, MD, Chief of Pediatric Neuroradiology
Asim F. Choudhri, MD, and Chief of Pediatric Neurology James Wheless, MD.
Le Bonheur and Semmes Murphey Neurosurgeon Nir Shimony, MD, says nearly 70% of patients treated by Le Bonheur’s epilepsy and brain tumor teams come from outside the Memphis area, including the Northeast, the Northwest and even Canada. These families seek out Le Bonheur for its reputation in handling the most complex cases combining seizures and brain tumors, often after being told elsewhere that treatment isn’t possible.
Many of these children have been living with frequent, debilitating seizures — sometimes 10 or more a day — because other institutions deemed intervention too risky, Shimony said. “We are willing to take the challenge and be very transparent with the family about what we can achieve from the very beginning. But I think that with our experience, we’re able to achieve a lot of success for those families who were told, basically, ‘just live with your seizures.’”
While exact national data on children presenting with both epilepsy and brain tumors is limited, these complex cases are a regular part of Le Bonheur’s work.
Shimony said seizures are very common in kids with brain tumors, especially low-grade tumors. Because not every kid with seizures will have a brain tumor, the seizures are often diagnosed, and epilepsy treatment started, far before the brain tumor is found. Tumors, when they do exist, will only be revealed with an MRI or CT scan, tests that unfortunately can come months after the original seizure diagnosis in some cases.
“From a treatment perspective, the easiest scenario is when a tumor is detected during the first Emergency Department visit that came after the first ever seizure episode,” Shimony said. “Usually, if you take care of the brain tumor, that will be it. But sometimes it’s more complicated. Kids may have very complex brain tumors and on top of that have very complex epilepsy. Those are the challenging cases coming to us a lot of the time.”
This is when the brain tumor and epilepsy team of teams is activated and why so many patient families find their way to Le Bonheur Children’s Hospital.
A Team of Teams
Shimony emphasized that this program is successful not because of any one doctor or specialty, but because of the team. The collaboration works, he says, only because the specialists, including all the entities they are associated with and all the hard-working administrative staff, are rowing in the same direction.
When it comes to neurosurgery, Le Bonheur has one of the largest pediatric surgical brain tumor programs in the country, powered by a unique partnership among Le Bonheur, Semmes Murphey Clinic, St. Jude Children’s Research Hospital and the University of Tennessee (UT) Health Science Center. Led by Le Bonheur and Semmes Murphey Neurosurgeons Paul Klimo, MD, MPH, chief of Pediatric Neurosurgery, and Shimony, the program is known for its aggressive surgical approaches and groundbreaking treatments.
Le Bonheur is also home to a comprehensive epilepsy program, accredited by the National Association of Epilepsy Centers as a Level IV center, the highest designation and one of only a few in the United States. Under the leadership of James Wheless, MD, chief of Pediatric Neurology, and Sarah Weatherspoon, MD, associate chief of Pediatric Neurology at Le Bonheur, the team consists of internationally recognized pediatric neurologists with a deep bench of knowledge and experience. Le Bonheur’s neurologists have access to advanced neuroimaging, diagnostics, clinical trials and emerging therapies.

While neurosurgery and brain tumors often fall under one domain and epilepsy under another, these complex cases blur the lines. At Le Bonheur, treatment for these patients is a unified effort between neurosurgery, for tumors, and neurology, for epilepsy. Surgical epilepsy cases require ongoing collaboration among neurology, neurosurgery, neuroradiology, neuropsychology and specialized labs such as transcranial magnetic stimulation (TMS) and magnetoencephalography (MEG). Without the input from the TMS and MEG teams and without the detailed input from the neuropsychology team, these complex surgeries would never have the same successful results.
The collaboration extends beyond Le Bonheur’s walls. For children with complex brain tumors and epilepsy, the team works closely with St. Jude Children’s Research Hospital in consultation and shared care. Together, they combine expertise in oncology, neurology, imaging and pathology to guide treatment decisions and improve outcomes, creating a level of care few institutions can match.
These two teams work closely with neuroradiologists, led by Asim Choudhri, MD, chief of Pediatric Neuroradiology, without whom accuracy and precision for these complex cases are not possible. This rounds out a medical force doing some of the most challenging work in pediatric medicine today.
Getting to Work
When a patient needs them, neurosurgery, neurology, neuroradiology and other experts meet to discuss their cases. But the details of these discussions begin with questions. Where are the seizures coming from? Which part of the brain is involved? Can we treat the tumor and the seizures at the same time? Do we need to stage operations — conduct several surgeries to solve both problems? From these questions, the team begins to tailor a patient’s treatment. And every team member knows, their work must be precise and delicate.
“A lot of these tumors reside in important areas of the brain that affect language, motor function or memory,” Shimony said. “So, it’s not as simple as just going in and removing tissue. In many of these complex cases, complete resection of the tumor is not possible, but the team still needs to find a way to elevate the quality of life of the patient and their families, by minimizing the residual tumor and finding a way to control the seizures by removing or interfering with the epilepsy network.”
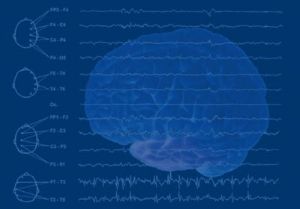
The team moves through a patient’s treatment in three major phases. In Phase I, the patient sees a neurologist and has an electroencephalogram (EEG) that measures electrical activity in the brain to look for areas involved with generating the seizures.
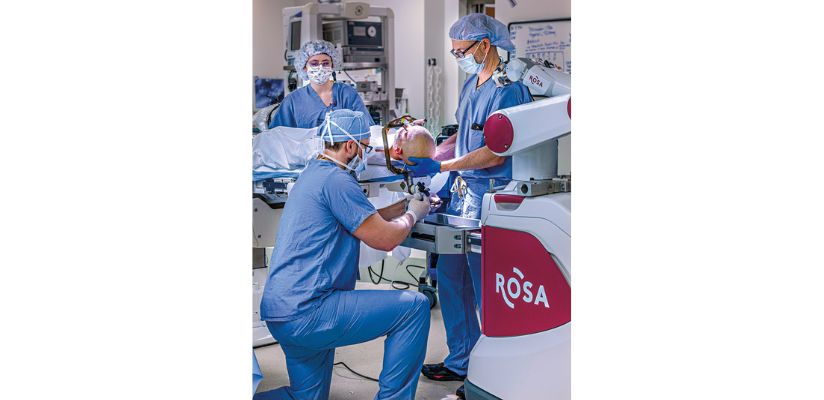
technology that can help place electrodes to determine seizure locations.
Testing continues in this phase to gather deeper information or put “bricks in the wall,” as Shimony says. These tests could include a neuropsychology evaluation, TMS or the advanced MEG system, used to identify important functional areas of the brain and plan surgeries for epilepsy and brain tumor removal.
Phase II fine-tunes all the discoveries made in Phase I. Surgeons use stereoencephalography (sEEG) (sometimes with other electrodes on the surface of the brain) to perform preliminary diagnostic surgery in which tiny electrodes, with a diameter of around 1 millimeter, are placed into the brain using a robotic surgery system. With these electrodes in place, doctors have a 3D map to see where seizures are being generated. From there, the doctors can devise the best plan for the needed surgical solutions.
“All these ‘bricks in the wall’ now show the final picture. We now have an advanced image of the brain, which helps me determine what I can and can’t take out, which path I can or cannot go through,” Shimony said. “You have to be very careful and know exactly where you are going in. The 3D map helps
us a lot.”
Phase III moves back into the operating room. The neuroradiology team is present in this stage to manage the intraoperative MRI (iMRI) and help guide surgeons through the procedure in real time. The neurology team is also present to monitor results, record brain activity directly from the brain and consult throughout the surgery. In the end, Le Bonheur surgeons will then activate the exact plan to help the patient, that might include removing the tumor or using a laser to destroy it, as well as intraoperative monitoring to make sure any epileptogenic tissue is removed to allow for best seizure control after surgery.
‘Ultimate Success’
The “ultimate success” in these cases, Shimony said, is no tumor and no seizures. Often, though, the outcome includes significant tumor eradication and ongoing epilepsy management. If the patient needs to continue treatment for epilepsy, but now his or her epilepsy is completely controlled, this is considered a big success and step towards better quality of life.
“The kid can continue in his or her life, followed periodically with MRI and maintenance medication,” Shimony said.

Help us provide the best care for kids.
Le Bonheur Children's Hospital depends on the generosity of friends like you to help us serve 250,000 children each year, regardless of their family’s ability to pay. Every gift helps us improve the lives of children.
Donate Now