Bringing Home a VAD
16-year-old Deshawn Bell landed at Le Bonheur’s doors in heart failure. He needed a ventricular assist device (VAD) to keep his heart beating. One hundred fifteen miles from his home in Tupelo, Miss., Deshawn and his family faced a long hospital stay while they waited for his body to regain strength while on VAD support.
Le Bonheur cardiologists quickly recognized that Deshawn was an ideal candidate for the Outpatient VAD Program – a new initiative from Le Bonheur’s Heart Institute that allows qualified patients to go home to recuperate with their VAD still implanted.
“Previously, if a patient had a VAD the only option was for them to stay in the hospital for the entire duration of implantation,” said Le Bonheur Medical Director of Mechanical Circulatory Support Mohammed Absi, MD. “Staying in the hospital for months is not good for a child’s quality of life, especially with chronic heart failure patients who have already been to the hospital many times.”
Seven weeks after VAD implantation, Deshawn was discharged from the hospital with his VAD to recover and rehabilitate in his own home with family and friends close by.
Thanks to this initiative, children and adolescents with a VAD can now have an improved quality of life and rehabilitate in the comfort of home, both of which lead to better outcomes for those who undergo heart transplant.
A Comprehensive Program

A VAD can be crucial to a child’s rehabilitation prior to heart transplant. Above, Le Bonheur Surgical Director of Pediatric Heart Transplant and the Ventricular Assist Device Program Umar Boston, MD, conducts a heart transplant surgery for a child previously on a VAD.
Le Bonheur’s VAD program was first established in 2016 in conjunction with the Cardiomyopathy, Heart Failure and Heart Transplant Programs. A VAD can provide the bridge to a heart transplant — allowing a child’s body the crucial time it needs to gain strength and heal from the effects of heart failure. VADs can also be a destination therapy if a child is not qualified for heart transplant.
“The primary goal of the VAD is for physical, nutritional and end organ rehabilitation, but another important factor prior to heart transplant is psychosocial rehabilitation,” said Umar Boston, MD, Le Bonheur’s surgical director of Pediatric Heart Transplant and Ventricular Assist Device Program. “If a child goes into transplant well rehabilitated, the outcome will be much better, but it can take a long time to get them to that state prior to transplantation.”
In order to provide the full rehabilitation that only the comfort of home can offer, Le Bonheur’s Heart Institute developed the Outpatient VAD Program that would allow select children with a VAD to be cared for in an outpatient clinic instead of an inpatient hospital stay. Using designs from the Advanced Cardiac Therapies Improving Outcomes Network (ACTION), Mechanical Circulatory Support Coordinator Amber Merritt, BSN, MSN, CCRN, and Heart Transplant and VAD Coordinator Tiffany Street, BSN, RN, worked to make this program a reality by developing the Outpatient VAD Clinic, protocols and caregiver education.

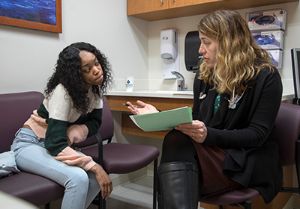
In order to go home with a VAD, families must be trained on how to care for the device daily and in emergency situations. Mechanical Circulatory Support Coordinator Amber Merritt, BSN, MSN, CCRN, and Heart Transplant Coordinator Tiffany Street, BSN, RN, provide this education to caregivers and the patient before leaving the hospital.
Patients must meet specific qualifications to go home with a VAD. Only fully implantable VAD devices can go home with a patient, and the patient must also be medically stable with good control of their heart failure symptoms. But qualifications aren’t just medical. The patient must have significant psychosocial and community support. This means that the family and patient are comfortable learning to care for the VAD, and the surrounding community — hospitals, schools, emergency departments — is on board and willing to be educated as well.
“This program allows us to provide all of the care any child with heart failure may need,” said Boston. “The goal is to provide a full service line to any child who has heart failure to optimize their care for the best outcomes.”
The Road Home
The discharge process with a VAD takes weeks and sometimes months, and is closely coordinated by Merritt and Street. A safe community at home is created for the patient by educating the local medical community on VAD implantation. Merritt works with electric companies to ensure the power will never be disconnected, coordinates with Pedi-Flite — Le Bonheur’s specialized transport for critically ill and injured children — in case of emergency transportation and designs a protocol for the local hospital for an emergent situation.
“It takes a whole village to make this possible,” said Merritt. “But we know from a psychological standpoint that the child needs to be at home.”
The patient and family members are trained for day-to-day VAD care and emergency procedures, learning to recognize and address signs of device malfunction. Caregivers learn everything from dressing changes to changing out batteries on the device. They are CPR-trained and must pass written and hands-on competency tests.
The final test for patients and families is an independent 24-hour hospital stay. During this time, the family provides all care for the patient without the intervention of nurses or physicians unless an emergency occurs.

Heart Institute patient Deshawn Bell visits the Outpatient VAD Clinic for follow-up with Le Bonheur Medical Director of Mechanical Circulatory Support Mohammed Absi, MD. Thanks to the Outpatient VAD Program, Deshawn is able to visit the clinic periodically for his care instead of staying in the hospital for the duration of his VAD implantation.
After discharge, the patient transitions across the street from the hospital at FedExFamilyHouse, where out-of-town families stay free of charge, for two weeks. They are seen every other day in clinic, continue to work with any outpatient rehab services they may need and remain close by the hospital for troubleshooting the VAD.
“FedExFamilyHouse allows us to provide a transitional phase to families before sending them home. It’s a blessing to have such a resource close to us,” said Absi.
After two weeks, the patient is typically ready to go home with their VAD. They are provided a 24/7 phone number for questions and emergencies and continue regular clinic follow-up at Le Bonheur with physicians, social workers, nutritionists and any other needed specialists.
From Diagnosis to Discharge: Outpatient VAD Program Timeline
Children must meet a variety of qualifications, including certain diagnoses, VAD type and other psychosocial factors, to go home with a VAD. This is the timeline of what the journey looks like.
Future Impact
Ultimately, Le Bonheur cardiologists believe that the Outpatient VAD Program will improve quality of life for the patients and their families as well as heart failure and transplant outcomes. Where previously patients spent months in the hospital, they will now spend that time of recuperation at home returning to as much of their usual routine and activities as possible. Le Bonheur physicians hope that the mental and physical benefits of being at home will go on to impact transplant outcomes.
“We expect to see improvement in terms of one-year and three-year survival,” said Boston. “Our hope is that they will go into transplant so well-rehabilitated, both physically and psychologically, that they will be able to handle all aspects of heart transplant much better.”
Meet Our Outpatient VAD Team
- Mohammed Absi, MD - Medical Director, Mechanical Circulatory Support
- Umar Boston, MD - Surgical Director, Pediatric Heart Transplant and Ventricular Assist Device Program
- Jeffrey A. Towbin, MD - Executive Co-Director, Le Bonheur Heart Institute
- Jason Goldberg, MD - Pediatric Cardiologist
- Jennifer Kramer, MD - Pediatric Cardiac Critical Care Intensivist
- Hugo Martinez, MD - Pediatric Cardiologist
- Kaitlin Ryan, MD - Pediatric Cardiologist
- Jenny Strelsin, MSN, PNP-AC - Pediatric Cardiology Nurse Practitioner
- Webb Smith, PhD - Cardiac Rehabilitation Exercise Physiologist
- Amber Merritt, BSN, MSN, CCRN - Mechanical Circulatory Support Coordinator
- Tiffany Street, BSN, RN - Heart Transplant and Ventricular Assist Device Coordinator
At Home with a VAD

Deshawn Bell, 16
Tupelo, Miss.
Before the Outpatient VAD Program, patients like Deshawn Bell would spend months in the hospital. After VAD implantation, they would rehabilitate inside the hospital walls until the device was removed or they underwent a heart transplant.
But thanks to the new initiative, Deshawn is now the first patient from Le Bonheur to be discharged with a VAD. He is at home with his family in Tupelo, Miss., healing and regaining strength.
“We knew that we could send Deshawn home safely,” said Mohammed Absi, MD, Le Bonheur medical director of Mechanical Circulatory Support. “Thanks to a lot of teamwork, especially work and effort from Deshawn and his family, we were able to make this a reality.”
Deshawn Bell came to Le Bonheur in a shock-like state, according to Absi, and was so sick that he required heart-lung bypass to survive. Diagnosed with congestive heart failure, he eventually was able to receive a VAD. Over time, his heart failure symptoms improved to the point that doctors could remove the VAD and manage his condition with medication.
But a second bout of heart failure called for the VAD to be re-implanted, this time for the long haul. Previously patients like Deshawn would spend months in the hospital. Instead, cardiologists determined that Deshawn and his mom, Kimberly, would learn how to care for the VAD themselves, so Deshawn could recuperate at home.
“We underwent an extensive teaching experience before returning home,” said Kimberly Bell. “We learned everything about the VAD from doing dressing changes to changing out the batteries.”
Mechanical Circulatory Support Coordinator Amber Merritt, BSN, MSN, CCRN, then went to Tupelo to meet with the local hospital and EMS system to refresh them on care of a pediatric patient like Deshawn and how to contact Le Bonheur in case of emergency. Once ready, Deshawn and Kimberly stayed at FedExFamilyHouse for two weeks where they were seen twice a week in clinic and continued outpatient services every day.
“FedExFamilyHouse gave us a step down before we get home, 115 miles away from the hospital,” said Kimberly.
Finally, they were able to return home to Tupelo where Deshawn resumed as many aspects of his normal routine as possible. Instead of spending months in the hospital, the Bell family visits the Outpatient VAD Clinic at Le Bonheur every few weeks for check-ups with his care team.
Help us provide the best care for kids.
Le Bonheur Children's Hospital depends on the generosity of friends like you to help us serve 250,000 children each year, regardless of their family’s ability to pay. Every gift helps us improve the lives of children.
Donate Now