Re-use of N95 Respirators
Shortages of N95 filtering face respirators led Le Bonheur researchers to partner with a local small business to develop a method of mass viral decontamination for N95s using a dry heat kiln at a pallet manufacturer. The research provided a design for a wooden container capable of mass reprocessing up to 12,000 N95s in an eight-hour period, as well as qualitative retained filtering efficiency and documentation of influenza A virus inactivation. A pandemic strain of influenza A virus was used to validate decontamination.
N95s are intended to be single-use, but when faced with critical shortages, N95 decontamination for re-use may be an option. Potential choices available for SARS-CoV-2 inactivation include dry or moist heat, vaporized hydrogen peroxide (VHP) and ultraviolet germicidal irradiation (UVGI).
“VHP received emergency FDA approval in this pandemic situation, but it requires costly specialized equipment,” said Le Bonheur Medical Director of Infectious Diseases Nick Hysmith, MD. “Heat treatment is an attractive alternative that is simple, accessible worldwide and relatively inexpensive.”
Dry heat kilns, such as those used to heat treat wood packaging material, are required to meet approved standards for products of international trade. Wood packaging material is required to achieve a minimum temperature of 56° C (132.8° F) for a minimum of 30 minutes. Because of this regulation, sawmills, pallet and crating manufacturers and third-party kiln companies are uniquely suited to substitute as decontamination chambers for repurposing N95s as they are distributed globally with large kilns for heat treatment.
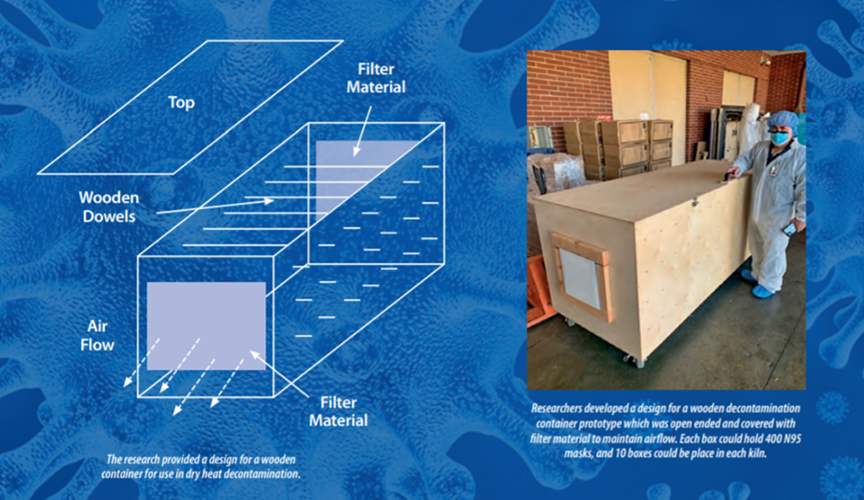
In this experiment, Le Bonheur researchers used a high-capacity piggy-back pallet kiln with a gas heating unit capable of producing dry heat up to 200° F. Researchers constructed a wood decontamination dry heat container prototype 4 feet wide, 8 feet long and 3 feet high that could hold up to 400 N95 masks. Each end of the box was open and covered with filter material to maintain airflow without allowing particulate matter to pass through. Fans inside the kiln ensured even heat distribution. Approximately 10 boxes could be placed within the 53-foot-long kiln.
Two H1N1 strains of influenza A virus were used to compare this effect of dry heat kiln treatment on a highly virulent laboratory strain versus a clinically relevant pandemic strain. Virus was added directly to the surface of N95s to mimic real world conditions. For testing, the kiln was programmed to heat to 73.88° C (165° F) for 35 minutes in order to inactivate the virus.
After heat treatment, both strains of influenza A were completely inactivated. The masks showed no observable material degradation, and each passed qualitative seal and fit-testing after reprocessing.
“This decontamination technique provides a cost-effective and readily accessible method of inactivating virus while also preserving filtering efficiency for up to six cycles, and potentially more,” said Hysmith.
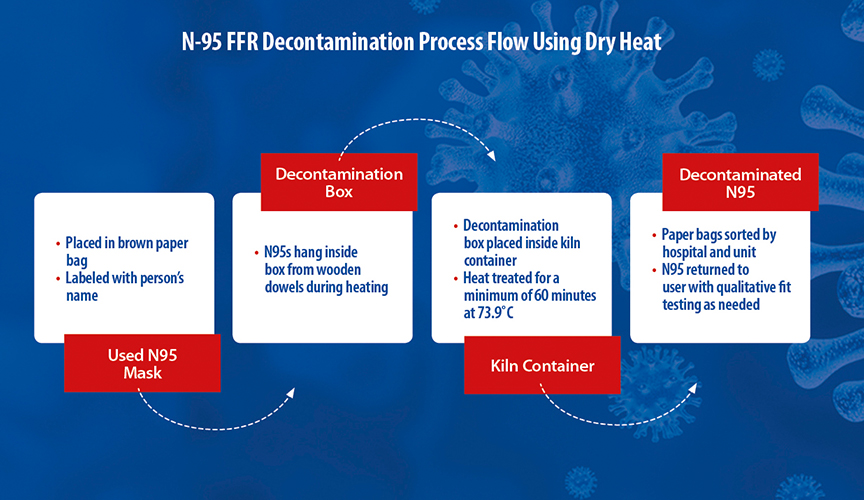
Using this method, nearly 12,000 N95s could be repurposed in an eight-hour period for a total approximate cost of $100.44 in energy consumption. Researchers also developed a hospital workflow that allowed repurposed masks to be returned to the original employee after reprocessing.
“This method will improve children’s health care by mitigating PPE shortages during pandemic situations and provide a widely accessible method of reprocessing that can be used by small or rural hospital networks,” said Hysmith.
Help us provide the best care for kids.
Le Bonheur Children's Hospital depends on the generosity of friends like you to help us serve 250,000 children each year, regardless of their family’s ability to pay. Every gift helps us improve the lives of children.
Donate Now