Center of Attention
Hospital-wide effort reduces CLABSI rate by 44%
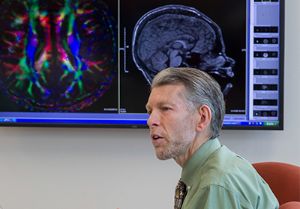
In 2017, Le Bonheur Children’s had 27 patients contract a central line-associated blood stream infection (CLABSI) during their hospital stay. Infectious Disease Specialist Nick Hysmith, MD, knew that this was 27 patients too many.
“Our standardized infection ratio was too high,” said Hysmith. “Patient safety and quality care is our top priority. It was time to develop new strategies for reducing bloodstream infections.”
Hysmith and his colleagues set a goal to reduce CLABSIs by 20%, beginning with the reduction of the overall number of central lines used across the hospital. In 2017, the central line standard utilization ratio, or number of patients with central lines, had reached one in four.
By forming a CLABSI Task Force and participating in research in tandem with Critical Care Intensivist Sachin Tadphale, MBBS, MPH, FAAP, and the Bright STAR Collaborative, Hysmith and his team improved patient safety by reducing CLABSIs by 44% over two years.
A Bold Stance
Hysmith’s first step was to form a CLABSI Task Force consisting of invested front-line providers from every unit and physicians from the Neonatal Intensive Care Unit (NICU) and Pediatric Intensive Care Unit (PICU) who make real-time decisions.
“Immediately, the task force began identifying the fastest ways to reduce the overall number of central lines as well as providing instruction on appropriate care for the lines that we absolutely need,” said Hysmith. “We needed to be bold in our approach to reduce CLABSIs.”
The CLABSI Task Force created a rigid criteria for utilization of central lines, including who should have them and when they are necessary. Physicians are now required to put in a daily central line order to document why the line is needed. The task force has also encouraged the use of peripheral IVs by changing tubing and the care of peripheral access points.

For those necessary central lines, the task force created education bundles on the insertion and maintenance of central lines with a goal of compliance above 90%. In addition, new products were investigated that might help mitigate the chance of infection.
Finally, an apparent cause analysis was conducted after every CLABSI event. Cause analysis served to reveal irregularities in patient care and other contributions to infection.
We needed to be bold in our approach to reduce CLABSIs.
“When a CLABSI does occur, we want to take the opportunity to learn from it,” said Hysmith. “With cause analysis we can narrow down why they happen and institute new policies to prevent them in the future.”
Practical Steps to Reducing CLABSI
Le Bonheur’s CLABSI Task Force implemented many new initiatives to lower the CLABSI rate including:
- Daily central line orders. Physicians are now required to document necessity of a central line on a daily basis.
- Chlorhexidine gluconate (CHG) baths. CHG baths are mandated for all patients in critical care areas (with the exception of the NICU) and patients on medicalsurgical floors with central lines.
- New central line techniques. Physicians developed a technique to put lines in lower on babies to avoid the line going into the diaper.
- Reduction in daily cultures. Previously patients on heart-lung bypass had daily cultures drawn from the line. This as well as other routine lab collection from central lines has stopped.
A Collaborative Effort
Patient safety and quality improvements don’t occur in a silo. Hysmith and Tadphale understood the importance of collaboration with other children’s hospitals around the country to reduce CLABSIs.
They joined a group of 15 hospitals as a part of the Blood Culture Improvement Guidelines and Diagnostic Stewardship for Antibiotic Reduction in Critically Ill Children, or the Bright STAR Collaborative. This multi-institutional quality improvement effort out of Johns Hopkins Children’s Center was created to optimize blood culture use in PICUs thereby lowering CLABSI risk.
“Any time you enter a central line for a blood culture you increase the risk of infection,” said Hysmith. “The Bright STAR Collaborative allowed us to share our efforts with other hospitals and learn from initiatives around the country.”
The Bright STAR Collaborative recently conducted a study surveying providers in the 15 PICUs that are part of the collaborative. The study aimed to assess the perceptions of current blood culture practices and identify potential barriers to reducing unnecessary cultures.
According to the study, in addition to the raised risk of infection unnecessary blood cultures cause harm to patients including excessive antibiotics, longer hospital stays and increased cost.
The survey revealed that the barriers to reducing unnecessary blood cultures included variation in blood culture decisions across PICU sites as well as a fear of missing sepsis. Respondents stated that they believed culture use is driven by fear and reflexive habits – diagnostic stewardship is critically needed for blood cultures.

A Dramatic Result
These efforts have already lowered the CLABSI rate at Le Bonheur Children’s. Overall blood cultures have been reduced by 66%, which lowers the risk of infection. And at the end of 2019, the CLABSI rate had dropped by 44% from 2017.
“Le Bonheur is forward-thinking in the consensus not to culture or access lines unless it is absolutely necessary. Now we can proudly say that we are ahead of the game in our safety record and buy-in from physicians,” said Hysmith. “We have the lowest blood culture rate of any center in the Bright STAR Collaborative. We are leading the way in keeping children protected from bloodstream infections.”
Results from the Bright STAR Collaborative Study
347 clinicians were surveyed in the 15 PICUs enrolled in the collaborative in order to explore typical blood culture practices, attitudes and beliefs as well as potential barriers to changing culture use. Results include:
- 86% believe cultures are ordered reflexively
- 90% of clinicians obtain cultures for any new fever PICU patients
- 71% report that physicians do not examine patients before ordering cultures
- 33% do not obtain peripheral cultures when an indwelling catheter is in place
- 64% sample multiple lumens of central venous catheters for new fever
Barriers to reducing unnecessary cultures include:
- 80% report a fear of missing sepsis
- 61% say that achieving standardization among different clinicians would be challenging
- Source: Woods-Hill CZ, Koontz DW, King AF, et al. Practices, Perceptions, and Attitudes in the Evaluation of Critically Ill Children for Bacteremia: A National Survey [published online ahead of print, 2019 Nov 6]. Pediatr Crit Care Med. 2019;10.1097/ PCC.0000000000002176. doi:10.1097/PCC.0000000000002176
Help us provide the best care for kids.
Le Bonheur Children's Hospital depends on the generosity of friends like you to help us serve 250,000 children each year, regardless of their family’s ability to pay. Every gift helps us improve the lives of children.
Donate Now